Enhancing Assessment: Sepsis
What is sepsis?
Sepsis, put simply, is a total failure of the body’s natural compensation mechanisms in response to a systemic, broad infection. Per the quick Sepsis Organ Failure Assessment metric’s page, sepsis is a state of “life-threatening organ dysfunction due to a dysregulated host response to infection” (qSOFA).
Sepsis begins with a source of infection that has allowed for pathogen to either enter the body or to colonize a body tissue. For instance, one of the most common causes for sepsis in older females is urinary tract infections, with urosepsis accounting for up to 31 percent of all sepsis cases (Dreger et al., 2015). Pressure ulcers in bed bound or disabled patients also make up a significant source of sepsis infections yearly (Sepsis Alliance, 2021). A variety of factors including sedentary lifestyles, polypharmacy presence, diabetes, peripheral vascular disease, and other pre-existing health conditions make up risk factors that make the development of sepsis more likely. EMS in particular often sees sepsis in the context of bedbound or disabled patients that develop a general illness at home and gradually decline until they’re in a septic states.
Pathophysiology of Sepsis
Previous research used to suggest that the cause of mortality and morbidity in sepsis was the infection itself. However, new research shows that it is actually the body’s own improper and dysregulated immune response that causes clinical sepsis. There is no specific pathogen or microbe that causes sepsis.
There are several stages to sepsis, with the least severe forms being chronic and continual over a period of time and the most deadly being full-blown, decompensated septic shock. We will cover much of this within this article.
Sepsis begins with the systemic inflammatory response (SIRS). This stage is defined by 2 or more symptoms that broadly indicate a bodily response to a state of infection. These symptoms include tachycardia, a febrile or hypothermic state, tachypnea, hypercapnia, and heightened white blood cell counts (Hotchkiss et al., 2016). This stage does not include end organ damage, but is a clinically significant finding when screening for sepsis.
Sepsis then progresses into severe sepsis and is a life threat. This is when the clinical emergency for EMS providers has begun, and is the start of most sepsis protocols nationwide. End organ damage has begun at this stage, with symptoms including shock symptoms, hypotension, altered mental status onset, and acidosis. Patients experiencing this stage of sepsis are usually febrile (or afebrile, depending on the body’s ability to compensate), may be hyperglycemic despite having no previous diabetic history, tachypneic, tachycardic, and show signs of fluid imbalances. Lab values are particularly important in this stage, as assessment of values such serum lactate, WBC count, creatinine, and BUN can provide important clinical insights and help in recognition.
Septic shock is the final stage of sepsis, and is a life threat. At this stage of sepsis, the body has failed in regulating its internal immune response. The body attempts to maintain vasoconstriction for an excessive amount of time, but fails in the end. While a variety of factors exist for why the body begins to fall into shock, it is likely cardiogenic. Following excessive time under metabolic stress, the body reaches critical levels of nitric oxide production as part of its compensatory mechanism. This nitric oxide prompts systemic peripheral vasodilation. Fun fact: nitric oxide has the same mechanism as nitroglycerin, which is similarly used to induce vasodilation in the case of acute coronary syndrome patients.
Patients in septic shock show classic shock symptoms including hypoxia, tachypnea, excessive ETCO2 readings, acidosis findings, hypotension/arterial hypotension, altered mental status, and cardiac dysrhythmias. In addition, patients will typically either have spiking fevers or be hypothermic. This will be discussed in more detail below.
Sepsis & Organs
Cardiovascular - We must remember that sepsis occurs primarily in vulnerable and medically fragile populations such as immunocompromised pediatrics and geriatric patients. These patients, by baseline, tend to have less robust cardiovascular systems and decreased ability to compensate.
In an attempt to compensate for the increased metabolic stress, the body undergoes several changes. Stroke volume increases, prompting subsequent increases in cardiac workload. At the same time, the body drops its systemic vascular resistance in order to facilitate a higher physiologic preload and maintain cardiac workload. The body does this in order to ensure that blood, oxygen, and inflammatory/immune proteins are able to reach the site of infection in adequate amounts.
In the process of compensating, the body in particular produces nitric oxide and undergoes oxidative stress as it tries to respectively maintain systemic vascular resistance, maintain vascular tone, and ensure adequate oxygenation. However, this will eventually fail. As a result of the excessive production of nitric oxide, the body undergoes peripheral vasodilation when the vessels reach maximal vasoconstriction and NO levels hit critical levels. This leads to blood pooling within the vessels and compromised circulation. Because of preload, afterload, and cardiac output increases, the right ventricle also begins to fail as the body enters a state of septic shock (. Remember - the right ventricle is extremely fragile in comparison to the left ventricle, and is primarily responsible for maintaining the low pressure, high compliance pulmonary circulation to ensure oxygenation.
Septic shock is ultimately an end state of hypoperfusion. As widespread peripheral vasodilation occurs, the body’s preload drops. This in turn compromises cardiac output. The amount of blood running through the pulmonary circuit drops, resulting in dropping SpO2 in addition to reductions in oxygen use at the cellular level (Fink, 2002). The topic is complex and still undergoing more research, but the general takeaway is that compromised cardiac output, widespread metabolic acidosis, hypoxemia, and impaired cellular oxygen use all contribute to the end stages of shock.
Why hyperglycemia? As we stated above, severe septic patients may show hyperglycemic blood glucose levels despite having no previous diabetic history. When the body undergoes any form of physiologic stress, it begins to dump catecholamines and efferent responses. This holds true for stages of sepsis. As the body mounts its immune response to the infection, catecholamines are released to assist in things such as maintaining vascular tone, increasing heart rate and cardiac contractility, and stir the body to”fight” the infection. Catecholamines are also responsible for the release of glycogen from the body’s muscular and liver stores, increasing glucose production generally, and raising blood glucose levels. This is part of the natural compensation mechanisms of the body. Glucose elevation alone without other findings for sepsis does not indicate sepsis or raise mortality rates (Bar-Or et al., 2019). It is a general finding with any many forms of severe metabolic stress or illness.
When an otherwise sick has nonspecific malaise symptoms and hyperglycemia, it should prompt further assessment for sepsis.
Lab values? Several lab findings are core for making sepsis diagnosis and treatment decisions in hospital. While point-of-care lab testing remains unable for most EMS systems, it is beneficial that providers have a working knowledge of lab values and what they mean in the context of sepsis.
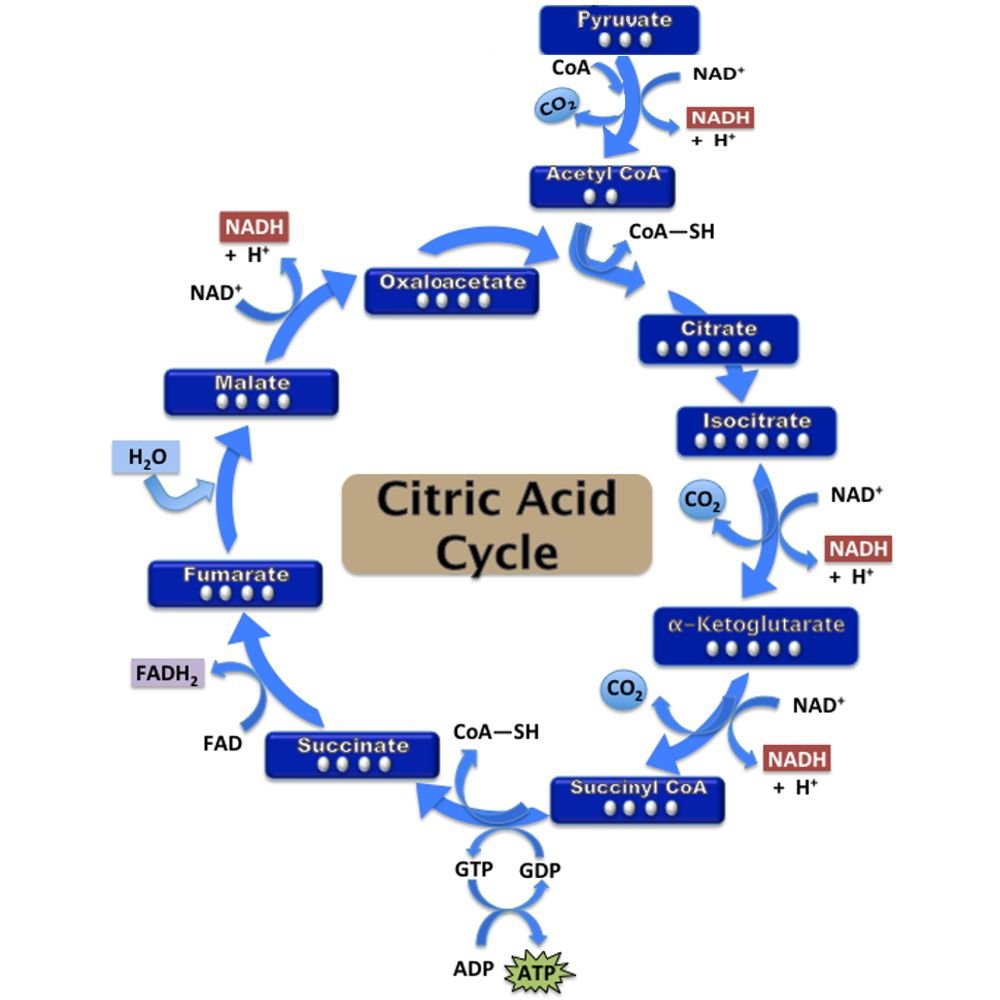
Lactate is the most commonly used lab value for sepsis diagnosis. The body uses 3 main metabolic pathways for the usual production of energy/ATP. These include glycolysis (the breakdown of glucose through food, naturally), the citric acid cycle (kreb’s cycle), and respiratory chain oxidation. The full extent of these mechanisms are too extensive to be discussed within this article alone, but it is important to note that lactate is primarily from the citric acid cycle. In the absence of oxygen, the body produces lactate as a byproduct of pyruvate metabolism in the the citric acid cycle. This process helps the body respond to anaerobic conditions, which end-stage sepsis has the potential to become.
Lactate is inherently acidic, and it’s clearance is inhibited during states of metabolic stress/organ failure such as sepsis. Because lactate is not cleared, it accumulates within the body uninhibited. This contributes to the acidotic state of sepsis. Serum lactate levels of over 2mmol/L in addition to other septic symptoms is diagnostic for severe sepsis, with 4mmol/L and above indicates a state of severe septic stage with end stage organ disease ongoing (Lee & An, 2016).
Both leukopenia (4000 or below WBC count) and leukocytosis (WBC count over 12000) can be indicative of sepsis when combined with other clinical findings (Tanaka et al., 2015). Leukocytosis is can result as the body spikes immune protein and WBC production in order to fight off the infection. Leukopenia can actually be a sign of a worse prognosis, as the body has failed in its ability to compensate with heightened WBC production. Leukopenia in a severely septic patient shows a failure of the body’s natural defenses.
Assessment & Treatment of Septic Patients
Assessment for sepsis should be more intensive in any patients that are members of vulnerable or medically fragile populations. Examples of such patients include bed bound patients, patients that had a prolonged downtime fall, organ transplant recipients, patients taking immunosuppressive drugs, patients with an immunodeficiency illness such as HIV/AIDS, and those with in-dwelling medical equipment such as tracheostomy tubes or implanted feeding tubes. Intravenous drug users that are young and otherwise appear healthy may have heightened risks for sepsis. Adults over age 65 are at the highest risk for sepsis out of any population (Sepsis Alliance, 2022).
Sepsis is most commonly the result of bacterial infections. Bed sores, surgical wounds, central lines, and open cuts are all common routes for bacteria to enter the body and cause infection. Sepsis can still result from any sort of pathogenic process, such as influenza or a pneumonia.
Important findings for sepsis assessment include:
Open or slow-healing bed sores
These are especially common in nursing homes, bed bound patients, or other long-term facilities.
Surgical wounds
Invasive surgical wounds require regular upkeep and cleaning.
Ask the patient about recent hospital admissions, surgeries, or doctor’s visits.
Diabetics have naturally impeded healing abilities and may be at increased risk of sepsis as a result.
“Track Marks” or sites of IV use
IV drug users often reuse old needles or share with one another. IV drug users are also unable to conduct quality assurance of drugs used. This increases the risk of sepsis exponentially in otherwise young, healthy patients.
UTIs/odors
Smell can be an important sense when assessing for possible sepsis findings.
A patient with a pungent urine odor may have an advanced UTI ongoing without other symptoms.
Patients that wear diapers regularly are at increased risk for sepsis and UTIs generally.
Clinical findings for sepsis include tachycardia, tachypnea, hypothermia or fever, hypotension, hypercapnia, hyperglycemia, and altered mental status. Patients in sepsis are often warm and flushed instead of having traditional pale, cold, and clammy diaphoretic skin that we usually expect in shock patients.
“Unexplained altered mental status in geriatric patients should greatly increase your suspicion for sepsis.”
Treatment of septic shock focuses heavily on fluid replacement/challenging. Septic patients are often dehydrated and fluid-depleted as part of the disease process, and may respond well to large fluid challenges. Fluid bolusing also helps decrease myocardial stress and improves preload. Lactate ringer’s fluids are ideal versus normal saline (0.9 percent) or other unbalanced fluids. Studies have shown that providing unbalanced fluids to septic patients or other patients with compromised excretory/renal function puts patients at increased risk of hyperkalemia and increasing acidosis (Kilic et al., 2020). Normal saline is already acidic with a pH of 5.5, while LR is closer to neutral at 6.5 pH (Davis, 2022).
Broad spectrum IV antibiotic administration is also crucial. Research indicates that administration of antibiotics within the first hour of sepsis identification and maintenance throughout care can prompt survival rates of up to 80 percent on average (Walchok et al., 2016). More EMS systems carrying broad spectrum antibiotics could help improve patient outcomes and save lives.
Beyond antibiotics and fluid resuscitation, chronotropic and inotropic agents such as Norepinephrine, Epinephrine, and Dopamine are used. These agents allow for the maintenance and support of blood pressure in a patient in severe septic shock. This helps in turn maintain mean arterial pressures, ensure tissue oxygenation and nutrition, correct hypoperfusion, and avoid the end organ damage that would otherwise occur when hypoperfusion causes ischemia.
Prehospital interventions for septic patients include large-bore vascular access for fluid and medication infusions. Patients should be provided cardiac monitoring including a 12Lead EKG to rule out other possible causes. End tidal monitoring should be performed continuously to assess acidosis states and how well the patient is compensating. Early notification and calling of a “sepsis alert” to the hospital is critical for ensuring handoff goes smoothly and the patient continues to receive the aggressive care they require once they are in the emergency department.
Works Cited
Bar-Or, D., Rael, L. T., Madayag, R. M., Banton, K. L., Tanner, A., Acuna, D. L., Lieser, M. J., Marshall, G. T., Mains, C. W., & Brody, E. (2019). Stress Hyperglycemia in Critically Ill Patients: Insight Into Possible Molecular Pathways. Frontiers in Medicine, 6. https://doi.org/10.3389/fmed.2019.00054
Davis, D. (2022). Ringer’s Lactate. In C. Kerndt & S. Singh (Eds.), StatPearls (2022 January ed., p. 1). StatPearls.
Dreger, N. M., Degener, S., Ahmad-Nejad, P., Wöbker, G., & Roth, S. (2015). Urosepsis—Etiology, Diagnosis, and Treatment. Deutsches Ärzteblatt International. https://doi.org/10.3238/arztebl.2015.0837
Fink, M. P. (2002). Cytopathic hypoxia: Is oxygen use impaired in sepsis as a result of an acquired intrinsic derangement in cellular respiration? Critical Care Clinics, 18(1), 165–175. https://doi.org/10.1016/s0749-0704(03)00071-x
Greer, J. (2015). Pathophysiology of cardiovascular dysfunction in sepsis. BJA Education, 15(6), 316–321. https://doi.org/10.1093/bjaceaccp/mkv003
Hotchkiss, R. S., Moldawer, L. L., Opal, S. M., Reinhart, K., Turnbull, I. R., & Vincent, J. L. (2016). Sepsis and septic shock. Nature Reviews Disease Primers, 2(1). https://doi.org/10.1038/nrdp.2016.45
Kilic, O., Gultekin, Y., & Yazici, S. (2020). <p>The Impact of Intravenous Fluid Therapy on Acid-Base Status of Critically Ill Adults: A Stewart Approach-Based Perspective</p> International Journal of Nephrology and Renovascular Disease, Volume 13, 219–230. https://doi.org/10.2147/ijnrd.s266864
Lee, S. M., & An, W. S. (2016). New clinical criteria for septic shock: serum lactate level as new emerging vital sign. Journal of Thoracic Disease, 8(7), 1388–1390. https://doi.org/10.21037/jtd.2016.05.55
Sepsis Alliance. (2021, November 30). Pressure Ulcers (Pressure Injuries). https://www.sepsis.org/sepsisand/pressure-ulcers-pressure-injuries/
Sepsis Alliance. (2022, March 17). Aging & Sepsis. https://www.sepsis.org/sepsisand/aging/
Tanaka, H., Ikeda, T., Ono, S., Suda, S., & Ueno, T. (2015). White blood cell counts have an impact on septic patient outcome followed by polymyxin-b immobilized fiber with direct hemoperfusion. Critical Care, 19(Suppl 1), P128. https://doi.org/10.1186/cc14208
Walchok, J., Lutz, M., & Pirrallo, R. (2016, August 31). South Carolina EMS Integrates Sepsis Care into Protocols. Journal of Emergency Medical Services. https://www.jems.com/patient-care/south-carolina-ems-integrates-in-hospital-sepsis-care-into-protocols/