Kidney Disease & The EMS Provider: The Basics
Per Center for Disease Control statistics, approximately 1 in 7 Americans suffer from some form of chronic kidney disease (CKD) (National Institute of Diabetes and Digestive and Kidney Diseases). For many, it remains a silent issue, with as many as 9/10 Americans having no knowledge of their chronic kidney disease (National Institute of Diabetes and Digestive and Kidney Diseases). Patients with CKD, especially those with advanced or end stage renal disease, are at high risk for adverse events and automatically become medically fragile patients in the context of surgeries/procedures, prehospital EMS care, and immunology.
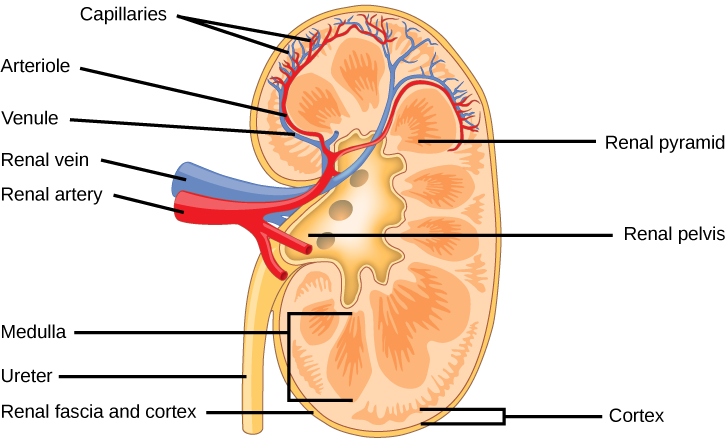
The Kidneys - A Review
The kidneys are located bilaterally in the upper quadrants. They are situated at the rear wall of the abdominal cavity and are not usually palpable through the skin. Kidneys are bean-shaped, with their concave side facing medially. A healthy kidney is approximately 5 inches long and weighs between 80 and 160 grams (Molina & DiMaio, 2012). Situated above the kidneys are the suprarenal glands - commonly known as the adrenal glands. These small glands are responsible for the excretion of the “fight or flight” catecholamines, including epinephrine and norepinephrine.
The kidneys are chiefly responsible for the filtration of the byproducts of metabolism out of the body and into urine. They are also responsible for the maintenance of fluid pressure and electrolyte balance in the body. This is accomplished through a variety of hormones and controlled protein regulation. The pituitary gland is the section of the brain primarily responsible for the control and regulation of kidney hormones.
Albumin - Albumin is the most common protein in blood circulation. It is made by the liver and has its excretion controlled by the kidneys in order to regulate fluid balance and osmotic pressure. Albumin “holds” water, and as a result is used by the body to regulate osmotic pressure and maintain fluid balance in body tissues. Albumin makes up 60 percent of vascular protein content, and is thus the primary means by which the body regulates fluid balances between the interstitial and vascular spaces (Garvovich et al., 2009).
Sourced from Lumen Learning.
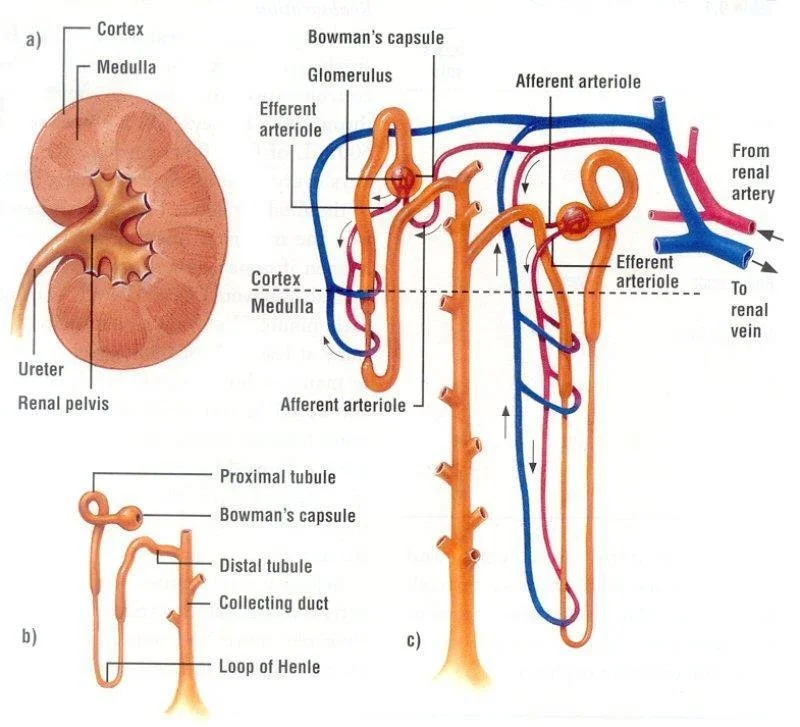
Sourced from ResearchGate
The kidneys are composed of functional units called nephrons. Nephrons are responsible for the filtration of urine and toxic substances. As fluid runs through the nephrons, it removes solutes in a controlled manner to maintain a desired solute concentration. For instance, the nephrons remove glucose from fluid as it runs through the tubules and returns it to circulation. The nephrons failing to remove adequate amounts of glucose would result in glycosuria - the condition of having abnormal amounts of glucose in urine. This is a significant clinical finding for diabetic patients.
Each nephron is made up of ducts and tubules as illustrated above. The vast majority of filtration is done in the proximal tubule, which is the first tubule seen in the diagram. Tubules of nephrons begin in the renal cortex and then run into the center pelvis of the kidney.
What is Chronic Kidney Disease?
Chronic kidney disease is a complex and multi-faceted disease process. In many ways, it is a blanket term to describe a decrease in renal efficiency and an inability to clear the usual toxins that are the kidneys are responsible for. Risk factors for the development of chronic kidney disease include hypertension, diabetes, generalized vascular diseases, obesity, and heart disease. These risk factors will be elaborated on in further detail throughout this article.
One core lab value - glomerular filtration rate - makes up the basis for much of the modern healthcare system’s screening techniques and is part of common lab panels. Glomerular filtration rate is used to estimate how much blood the kidneys filter in a short period of time. A GFR value over 60 is classed as normal. Values under 15 indicate renal failure, with values in-between indicating disease.
Glomerular filtration rate is often the first value that is found to indicate kidney disease, and is later used to chart its progression over time. Kidney disease is largely based on managing symptoms and attempting to prevent further injury. While some decrease in kidney efficiency is expected as part of the normal aging process, chronic kidney disease can progress to the point of requiring dialysis to sustain life.
It is important to note that chronic kidney disease (CKD) is different from acute kidney injury (AKI). Acute kidney injury is a state of damage to the kidneys that can progress into chronic kidney disease in time. Examples of etiologies that can cause acute kidney disease include sepsis, hypoperfusion as part of trauma, and some toxic drug overdoses.
Risk Factors for Chronic Kidney Disease
Risk factors for chronic kidney disease development share many commonalities with coronary artery disease/heart disease risk factors. We will explore some of the most prominent ones below.
Hypertension
Hypertension, in addition to causing vascular damage, causes damage to all tubules of nephrons. With time, unabated hypertension causes enough vascular damage to entirely destroy nephrons, thus reducing the efficiency of the kidneys and impacting their ability to reabsorb solutes.
Hypertension also worsens blood flow in the afferent arteries and arterioles that supply the kidneys with blood. By damaging these vessels, the blood supply to the kidneys is reduced with time. Hypertension significantly increases rates of chronic kidney disease.
Current clinical guidelines aim for systolic blood pressure averages under 130mmhg (Ku et al., 2019). This is done often with dietary and lifestyle changes in addition to medication management.
Because of the likelihood for medication management to maintain blood pressure, it is important to review medical history and current medications when dealing with a CKD patient.
Common medications to look for include beta blocker medications such as metoprolol or atenolol, calcium channel blockers, and ACE inhibitors (Ku et al., 2019).
Obesity
Obesity is a risk factor for the vast majority of health conditions. In addition to worsening conditions such as hypertension and increasing the risk for vascular damage, it also has a direct effect on the efficiency of the kidneys in removing solutes from circulation.
Obese patients have increased intraglomerular pressure, and thus do damage to their nephrons over time (Kovesdy et al., 2017). In combination with hypertension, this decrease in nephron function over time worsens kidney function and reduces glomerular filtration rate.
Obesity also increases the risk for diabetes.
Diabetes
Diabetes primarily plays a role in renal failure/CKD by way of vascular damage. As diabetes progresses and states of hyperglycemia are uncontrolled, renal blood supply is damaged.
Dialysis - What You Need to Know
The primary treatment for end stage renal disease is dialysis. Dialysis is essentially a full replacement for the normal solute filtration abilities of the kidneys. There are two ways that dialysis is commonly performed.
Peritoneal Dialysis involves the placement of a catheter into the peritoneal lining of the abdomen. A fluid called dialyzate is circulated into the peritoneal cavity. Dialyzate has lower concentrations in some solutes, such as magnesium, in order to allow for an osmotic gradient to be formed between the dialysis patient’s blood and the fluid inside the peritoneal cavity. Because the dialyzate fluid is lower in some substances, the osmotic pressure forces solutes to be exchanged between the circulating blood and dialyzate until the solute concentrations reach equilibrium on both sides. As a result, excess ions are removed from circulation just like functional kidneys would. The dialyzate is dumped out when the procedure is done.
Hemodialysis is a more common yet invasive form of dialysis. Hemodialysis involves the placement of a catheter or fistula into the arm or chest and then connection to an actual external machine to facilitate filtration. Hemodialysis also uses dialyzate. The process of dialysis is fine tuned to each individual patient according to their needs - some patients may require more fluid removal or different concentration dialyzate versus others.
Hemodialysis patients typically receive dialysis 3 days a week on a set schedule. Example schedules into Monday, Wednesday, Friday or Tuesday, Thursday, Saturday. Dialysis helps patients keep their solute concentration close to normal physiologic levels and maintain adequate fluid balance.
Prehospital Emergency Medicine & Dialysis Patients
While modern protocols are not necessarily fine tuned to any one specific patient population like CKD patients, it is important to think critically when dealing with CKD and dialysis patients. Taking care and providing care tailored to these patient’s complicated conditions can help reduce patient mortality and morbidity, decrease hospital stay lengths, and overall aid these patient in achieving good health outcomes.
Medication Administration
It’s important to be cautious when dosing and providing medications to CKD patients. A large amount of common drugs are primarily excreted and processed by the renal system, meaning that CKD patients are at higher risk of complications when receiving otherwise normal doses. Because of the decreased GFR seen in CKD patients, repeat doses of medications at regular intervals can build up to toxic levels while those same doses would be perfectly within the therapeutic range for patients with functioning kidneys.
For EMS providers, always consult your protocols when choosing to make dosing decisions. Dosing for ESRD patients may need modification. When possible, opt for lower dose ranges if available. It is important for all healthcare providers to provide a full assessment and understand the pathophysiology behind the medications they provide. Common medications that can be particularly taxing to CKD/ESRD patients include NSAIDs of all kinds, antibiotics, and antacids (National Kidney Foundation). Medications that disrupt the normal electrolyte balance of patients such as antacids require special monitoring in CKD patients as they have a reduced buffer to otherwise normal changes in acid-base balance.
Ketorolac, a common medication in prehospital medicine for inflammation-based abdominal pain, is an especially relevant medication to understand when it comes to treating CKD patients. Patients with ESRD/CKD that meet criteria to receive Ketorolac may require additional monitoring, lower dose ranges, or a different medication choice.
It is also important to note that accessing dialysis ports and fistulas is an inherently high risk procedure. Kidney patients are already at high risk of infection because of the etiology of their disease, and a potential route for infection is created with each access. Avoid accessing an implanted chest port, if possible, unless a severe emergency requires it.
Electrolyte Balance
Because CKD patients have reduced renal ability, they have severe difficulty in regulating electrolyte balance on their own. For instance, patients with renal failure are often advised to avoid high protein foods because of the excess demand protein places on the kidneys. CKD patients are also routinely advised to reduce consumption of or cut out high potassium foods such as bananas, apricots, or yogurt (National Kidney Foundation).
This failure to regulate electrolyte balance has significant impact on prehospital emergencies. ESRD patients commonly develop hyperkalemia - an excess of potassium. Potassium plays a critical role in the sodium-potassium ion pump, which is the mechanism responsible for regulating muscular depolarization and is essentially pertinent to heart health. Hyperkalemia is especially common in patients that have gone without dialysis for multiple days. A full article on hyperkalemia and EKG findings by EMSAware can be found here.
Prehospital management of electrolyte disorders is focused on prompt recognition and life support. Patients with electrolyte imbalance issues such as hyperkalemia may benefit from the administration of high dose albuterol, calcium chloride, insulin, and sodium bicarbonate as a means to mediate hyperkalemia-induced metabolic acidosis and remove excess potassium.
It is important to note that potassium and magnesium levels are heavily related. Hypomagnesemia is very commonly seen with hypokalemic patients - and vis versa (Hudali & Takkar, 2015).
Aneurysm Development & Hemorrhage
Hemodialysis involves repeat and regular access into fistulas. Repeat trauma from cannulations can prompt tissue damage over time, and in turn develop into an aneurysm in time. Fistula access should only ever be attempted by trained access staff. Aneurysms are a common cause for potentially life threatening bleeding in dialysis. It is critically important that providers recognize life threatening bleeds in dialysis patients and also educate patients on basic bleeding control in the event of rupture.
Mental Health
Patients with often chronic kidney disease/ESRD often describe feeling doomed by their condition. This is especially true for CKD patients with poor health literacy, poor access to regular dialysis and renal care, and poor home support systems. Suicide and self harm is a considerable issue with renal failure patients. Healthcare providers of all backgrounds should devote additional attention to addressing the mental health needs of CKD patients and being proactive in getting patients connected with community resources.
Works Cited
5 Drugs You May Need to Avoid or Adjust if You Have Kidney Disease. (2021, December 21). National Kidney Foundation. https://www.kidney.org/atoz/content/5-drugs-you-may-need-to-avoid-or-adjust-if-you-have-kidney-disease
Chen, Y., Zelnick, L. R., Hoofnagle, A. N., Yeung, C. K., Shireman, L. M., Phillips, B., Brauchla, C. C., de Boer, I., Manahan, L., Heckbert, S. R., Himmelfarb, J., & Kestenbaum, B. R. (2020). Prediction of Kidney Drug Clearance: A Comparison of Tubular Secretory Clearance and Glomerular Filtration Rate. Journal of the American Society of Nephrology, 32(2), 459–468. https://doi.org/10.1681/asn.2020060833
Garvovich, M., Zocco, M., & Gasbarrini, A. (2009). Clinical use of albumin in hepatology. Blood Transfus. https://doi.org/10.2450/2008.0080-08
Hudali, T., & Takkar, C. (2015). Hypocalcemia and hyperkalemia during magnesium infusion therapy in a pre‐eclamptic patient. Clinical Case Reports, 3(10), 827–831. https://doi.org/10.1002/ccr3.356
Kovesdy, C. P., Furth, S. L., & Zoccali, C. (2017). Obesity and Kidney Disease. Canadian Journal of Kidney Health and Disease, 4, 205435811769866. https://doi.org/10.1177/2054358117698669
Ku, E., Lee, B. J., Wei, J., & Weir, M. R. (2019). Hypertension in CKD: Core Curriculum 2019. American Journal of Kidney Diseases, 74(1), 120–131. https://doi.org/10.1053/j.ajkd.2018.12.044
Molina, D. K., & DiMaio, V. J. (2012). Normal Organ Weights in Men. American Journal of Forensic Medicine & Pathology, 33(4), 368–372. https://doi.org/10.1097/paf.0b013e31823d29ad
National Institute of Diabetes and Digestive and Kidney Diseases. (2021, December 9). Kidney Disease Statistics for the United States. https://www.niddk.nih.gov/health-information/health-statistics/kidney-disease