Medication Review: All About Epinephrine
Introduction
Epinephrine, colloquially known as the “hero hormone,” is a naturally produced hormone within the body. Produced by the suprarenal glands of the endocrine system, it is released in cases of “fight or flight” in response to innervation by the sympathetic nervous system. Along with norepinephrine, it is responsible for the body amping up its reaction to potentially dangerous stimuli and preparing for action. Over time, it has come through as a core emergency medicine tool. It uses a variety of different mechanisms to produce it desired action in patients.
Epinephrine first came into medical use in 1905, when it was used for demonstrating cerebral vasoconstriction by physiologist Carl Wiggers (Greer, 2015). From then, it expanded into further widespread use by the medical world. By the 1987, the FDA had approved the first commercial “EpiPen” device, bringing quick acting Epinephrine into the hands of regular people everywhere (Rimler, 2020). While modern day concerns over pricing exists, the fact remains - Epinephrine is a life saving, core drug in emergency medicine with a plethora of uses.
There are other uses for epinephrine beyond what is listed here - for instance, it often serves as a preoperative medication for reducing bleeds because of vasoconstrictive properties. This article is primarily intended to cover the most common EMS uses.
The Mechanism of Epinephrine
Epinephrine, otherwise known as adrenaline, is a natural body-produced hormone. As stated above, it is produced by the suprarenal glands under control of the sympathetic nervous system in response to fight or flight conditions. It is a sympathetic catecholamine - putting it in the same class of sympathetic neurotransmitters as norepinephrine and dopamine. It is an adrenergic agonist - meaning it works on the adrenergic receptors throughout the body. It works on both beta and alpha receptors are present in varying locations throughout the body and are responsible for producing actions within the body when stimulated. Medications can be either agonists - meaning they activate the receptors - or antagonists, meaning they block the receptors from activation by other agonists. Epinephrine is an agonist medication.
By working on beta-1 receptors, it is both chronotropic and inotropic for the heart. It increases contractility and spikes heart rate to increase blood flow. By acting on beta-2 receptors, epinephrine reverses bronchoconstriction and bronchodilates, allowing for increased oxygen exchange. It also prompts glycogenolysis and begins using glycogen stores within the liver to increase the available glucose the body has to work with. This is why extreme stress levels can sometimes spike blood glucose levels.
In the vasculature of the body, it acts on alpha and beta receptors to cause widespread vasoconstriction, raising blood pressure and increasing perfusion throughout the body. In some does, however, it is used for vasodilation - the opposite effect. In the doses that EMS commonly uses, it is almost solely used for vasoconstriction to support adequate pressures.
It additionally inhibits the parasympathetic nervous system, deprioritizing blood flow to the GI system and digestion. Essentially, epinephrine tones down any “relax” portion of the body and prioritizes the fight or flight response.
Uses of Epinephrine
Anaphylaxis
Anaphylaxis is a systemic overreaction to a detected allergen by the body. Classic signs and symptoms include urticaria, wheezing lung sounds, angioedema, abdominal pain or cramping, warm, hot flushed skin, a feeling of impending doom, itching (pruritus), hypotension, and tachycardia. EMS systems typically have a chart or set of symptoms in their protocols differentiating between a mild, moderate, and anaphylactic allergic reaction. Anaphylaxis is an immediate life threat. In anaphylaxis, epinephrine is provided in a 1:1000 (1mg/mL) ratio via IM means.
The most common allergens are peanuts, tree nuts of any kind, some medications (penicillin, for instance), and shellfish. They can also be environmental, including bee stings and animal bites. This list is not exhaustive - anaphylaxis can even be exercise-induced (NCATS).
In response to the detected allergen, the body goes into a state of shock. The body causes a dump of histamine, which acts on H1 and H2 receptors to provide many of the body’s allergic reaction effects. H1 receptors are primarily responsible for capillary permeability increases, while H2 receptors cause decreased GI motility and digestion. The body bronchodilates, resulting in airway constriction and wheezing. Laryngeal and airway edema can occur, blocking off the already constricted bronchioles and halting respiration. Peripheral vasodilation can cause massive fluid shifts out of central circulation, causing edema and hypotension. Increased capillary permeability aids this hypotension. This causes a significant drop in perfusion and drops the body into a state of hypoperfusion. If left untreated, anaphylaxis can progress into respiratory arrest and eventually cardiac arrest. Anaphylaxis is not a self correcting illness and requires care in all cases.
Epinephrine is given in the context of anaphylaxis as a “shock” to almost every adrenergic receptor in the body. By acting on beta-2 receptors, epinephrine reverses the bronchoconstriction that serves as the primary life threat. The body’s fight or flight response acts against the parasympathetic system, prompting the bronchioles to dilate to allow for more oxygen exchange and air flow. Epinephrine also acts on alpha and beta receptors throughout the vasculature to vasoconstrict and restore perfusion. The chronotropic and inotropic effects help the body return to a state of adequate perfusion.
Epinephrine can also be used as a vasopressor in anaphylactic shock in a drip form. The primary goal of this use is to raise blood pressure and increase arterial pressure as the patient recovers from the state of shock. This use is covered later on in the article.
Cardiac Arrest
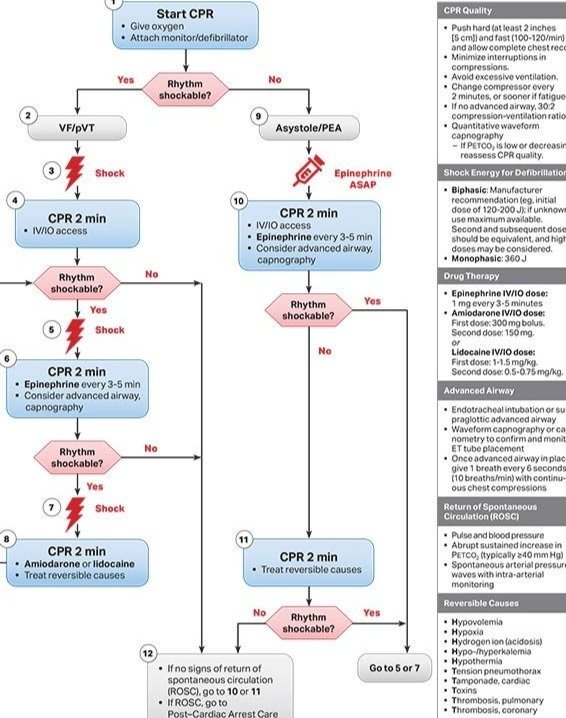
ACLS cardiac arrest algorithm sourced from American Heart Association.
AHA guidelines call for epinephrine to be provided every 3-5 minutes during cardiac arrest. In the real world, this translates to every-other 2 minute CPR cycle. Unlike other cardiac arrest medications, epinephrine is not a dysrhythmic - rather, it works to assist regaining perfusion throughout the body in addition to the manual compressions restarting circulation. It is the main drug involved in cardiac arrest management, and the only drug used in the case of nonshockable rhythms. As stated above, epinephrine increases myocardial contractility, jumps heart rate, and causes vasoconstrict - all of which assist the body in reversing from a state of hypoperfusion and restoring perfusion. Current studies debate the long-term benefits of epinephrine in cardiac arrest survival rates, but it remains in AHA ACLS algorithms to this day. Use of epinephrine in cardiac arrest is an ALS level procedure. It can be administered via intravenous or intraosseous means in a 1:10,000 (0.1mg/mL) ratio.
Asthmatics
Epinephrine can be used as a treatment for patients experiencing an asthma attack because of its profound effects on beta-2 receptors. Asthma attacks are ultimately an issue of severe, continuing bronchoconstriction. By providing epinephrine in the case of an asthma attack, EMS providers are able to reverse the bronchoconstriction and induce bronchodilation instead. Epinephrine is typically reserved for only the most severe, life threatening asthma attacks and is often combined with other treatments like Albuterol nebulizers. Asthmatics typically receive the same dose that anaphylaxis patients receive, but consult your own jurisdictions protocols for more information.
Hypotension
Epinephrine is commonly provided as a vasopressor in drip form if other means of fluid resuscitation and pressure support fail. The most common, AHA recommended dose is 2-10mcg/min, starting at 1mcg/min. Paramedics in the field may titrate the amount of infused epinephrine to achieve the desired response in pressure. Epinephrine is also included in drip form for combatting bradycardia. It achieves both increased heart rate and contractility by acting on beta-1 and alpha receptors as discussed above.
As with most forms of shock, a mean arterial pressure of 65 is considered the target prehospital, especially post-cardiac arrest. AHA guidelines at this time endorse permissive hypotension post-arrest.
Croup
Croup is an upper airway respiratory condition most commonly found with patients 3 months old to 3 years old. It can be found in older patients, but it is unlikely. It is largely a seasonal condition and occurs throughout the winter most commonly. It is viral in nature and its incidence often coincides with influenza seasons (Bjornson and Johnson, 2013). Symptoms usually resolve on their own, but severe cases can present an airway obstruction threat and require EMS attention.
Signs and symptoms of severe croup including worsening oxygen saturations, respiratory distress, a harsh “seal-like” or “whooping” cough, stridor, and high fevers. Severe croup develops into an airway threat because it can cause upper airway edema due to the localized viral infection present. This narrows the airway and reduces the effectiveness of respirations. If a patient with croup is overly agitated, this can increase oxygen demand and worsen respiratory distress.
Epinephrine has become the primary means for EMS providers to treat croup-induced airway threats in the field. It is used off-label in a nebulized form. Different EMS jurisdictions differ - check your own jurisdiction’s protocols for more information.
A Note About Beta Blockers
Beta blockers - as the name suggests - are beta receptor antagonists. They specifically function on the beta-2 receptors of the heart, reducing the heart rate and thus reducing cardiac workload. As a result, they are common in patients with hypertension. Many geriatric patients are also often prescribed beta blockers. Some younger patients may be prescribed propranolol specifically for anxiety conditions and panic attack control (Malka, 2021).
Because beta blockers effectively block any further agonists on the beta receptors, it can inhibit the action of epinephrine in the case of anaphylaxis. At higher doses, its effect is worsened. It is important for EMS providers to perform full assessments of both the patient and the scene to understand the role that beta blockers may play in treating their patient. Beta blockers will also reduce the ability of patients to compensate naturally in states of threatened hypoperfusion - they cannot adequately adjust their heart rate and contractility to meet the demands of the physiologic stress.
Patients who have taken high doses of beta blockers and are experiencing anaphylaxis or asthma attacks may require glucagon administration for epinephrine to be effective. You may require medical consultation for authorization for this unless it is a clear overdose (even so, some jurisdictions require consult in the case of clear overdose). Beta blocker use is something to consider with anaphylaxis/asthma patients refractory to epinephrine.
Additional Reading
JointEMSProtocols - Epinephrine
PharmacyTimes - Dangers of Beta Blockers + Epinephrine
This article was written off the author’s own pre-existing knowledge. Specifically cited sources were used for any gaps in knowledge and draw off insights from current research.
Works Cited
Arthur, Greer. “Epinephrine: A Short History.” The Lancet Respiratory Medicine, vol. 3, no. 5, 2015, pp. 350–51. Crossref, https://doi.org/10.1016/s2213-2600(15)00087-9.
Taylor BN, Cassagnol M. Alpha Adrenergic Receptors. [Updated 2021 Jul 13]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK539830/
“Exercise-Induced Anaphylaxis | Genetic and Rare Diseases Information Center (GARD) – an NCATS Program.” National Center for Advancing Translational Sciences, rarediseases.info.nih.gov/diseases/6392/exercise-induced-anaphylaxis. Accessed 1 Jan. 2022.
Bjornson, Candice L, and David W Johnson. “Croup in children.” CMAJ : Canadian Medical Association journal = journal de l'Association medicale canadienne vol. 185,15 (2013): 1317-23. doi:10.1503/cmaj.121645
Malka, Sarhah. “Propranolol For Anxiety: Can Beta Blockers Help?” K Health, 19 Oct. 2021, https://khealth.com/learn/anxiety/propranolol/.
“2020 American Heart Association Guidelines for CPR and ECC.” Cpr.heart.org, American Heart Association, https://cpr.heart.org/en/resuscitation-science/cpr-and-ecc-guidelines.